Slide 1
Good afternoon one and all. This is Dr. Salma post graduate 2nd year from the department of general medicine. Today we will be trying to relate to the pain suffering of one our patient who had travelled from West Bengal to get relieved of her pain.
Slide 2
The patient had travelled from West Bengal to narketpally as she had been suffering from pain in the right hypochondrium and pelvis radiating to the back since the past 2 months. Also had complaints of pain in the left hypochondrium and loin since the past 15 days. The pain was continuous, no aggravating or relieving factors were noted. For the pain she was given inj. Buscopan and was asked to get a usg abdomen done.
Slide 3The patient had travelled from West Bengal to narketpally as she had been suffering from pain in the right hypochondrium and pelvis radiating to the back since the past 2 months. Also had complaints of pain in the left hypochondrium and loin since the past 15 days. The pain was continuous, no aggravating or relieving factors were noted. For the pain she was given inj. Buscopan and was asked to get a usg abdomen done.
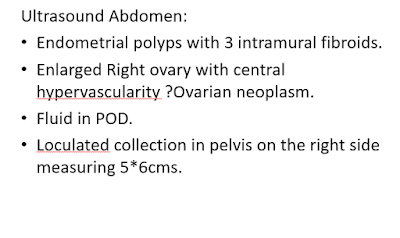
Ultrasound abdomen revealed a endometrial polyp and intramural fibroid. Enlarged right ovary with central hypervascularity.possibility of ovarian neoplasm.
Slide 4
MRI pelvis was done the same day which revealed an enlarged right ovary with a heterogeneous lesson with solid component and small cystic area. A long vascular pedicle to the right ovary was also noticed. She was operated on the same day. An emergency laprotomy was done with right salpingoophhorectomy and left ovarian drilling.
MRI pelvis was done the same day which revealed an enlarged right ovary with a heterogeneous lesson with solid component and small cystic area. A long vascular pedicle to the right ovary was also noticed. She was operated on the same day. An emergency laprotomy was done with right salpingoophhorectomy and left ovarian drilling.
Slide 6
Postoperatively she was started on inj. Tramadol 8th hourly for the pain and a referral was put to us in view of abnormal breath sounds and for hypotension. The case was then taken up by our department for further management. She was started on ionotropic support for her hypotension.
Postoperatively she was started on inj. Tramadol 8th hourly for the pain and a referral was put to us in view of abnormal breath sounds and for hypotension. The case was then taken up by our department for further management. She was started on ionotropic support for her hypotension.
Slide 7
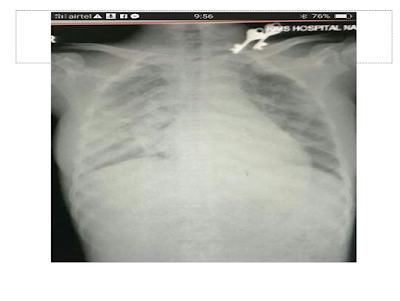
Her ionotropic support was gradually weaned off and her blood pressure was maintaining around 120-130/90 mm Hg without ionotropic support. But she still complained of pain abdomen and a pleuritic chest pain so we had added Tab. Ultracet 6th hourly to maintain the analgesic effect. This is her x-ray which showed patchy infiltration in the chest. A pulmonology opinion was taken and in addition to our previous findings, the pulmonary PG found a few significant cervical lymph nodes that we had missed on our initial evaluation. They had advised for a sputum for AFB and pleural fluid aspirate and an fnac of the cervical lymph node.
Her ionotropic support was gradually weaned off and her blood pressure was maintaining around 120-130/90 mm Hg without ionotropic support. But she still complained of pain abdomen and a pleuritic chest pain so we had added Tab. Ultracet 6th hourly to maintain the analgesic effect. This is her x-ray which showed patchy infiltration in the chest. A pulmonology opinion was taken and in addition to our previous findings, the pulmonary PG found a few significant cervical lymph nodes that we had missed on our initial evaluation. They had advised for a sputum for AFB and pleural fluid aspirate and an fnac of the cervical lymph node.
Slide 8
In the meanwhile with our ongoing struggles to find out the reason for the patchy infiltrate in the chest whether a disseminated Tuberculosis or a disseminated malignancy we were nowhere near the diagnosis of the ovary sample which had been sent for the histopathology report.
Slide 10 11
The patient continued to have the fever spikes despite on IV antibiotics and the pain seemed not to reduce. She still had persistent pain despite a fentanyl patch, tramadol and Ultracet
Slide 12
In the meanwhile, the CT chest showed pleural effusion and mediastinal lymphadenopathy. 2nd fentanyl patch was applied.
In the meanwhile, the CT chest showed pleural effusion and mediastinal lymphadenopathy. 2nd fentanyl patch was applied.
Slide 13
This is the slide picture of the fibrothecoma component of the right ovary which we had attained on our visit to the pathology department for the histopathology opinion of the specimen sent.
This is the slide picture of the fibrothecoma component of the right ovary which we had attained on our visit to the pathology department for the histopathology opinion of the specimen sent.
Slide 14
We had got a CecT of the chest and abdomen done to note the dissemination if present as we were wiser now with the histopathological diagnosis of the malignant fibrothecoma. This is the CecT picture of the chest which shows the involvement with the probable dissemination of the malignant fibrothecoma into the mediastinal lymph nodes.
We had got a CecT of the chest and abdomen done to note the dissemination if present as we were wiser now with the histopathological diagnosis of the malignant fibrothecoma. This is the CecT picture of the chest which shows the involvement with the probable dissemination of the malignant fibrothecoma into the mediastinal lymph nodes.
Slide 15 and 16
By the time we had come to the histopathological diagnosis of the malignant fibrothecoma we had searched on to find whether we could get any similar case reports of a malignant fibrothecoma with dissemination into the lymph nodes. We found a similar article of a 50-year-old postmenopausal lady with a leutinising thecoma and sclerosing peritonitis. But our patient had involvement of lymph nodes and probably even the sclerosing peritonitis which aptly explains her pain.
By the time we had come to the histopathological diagnosis of the malignant fibrothecoma we had searched on to find whether we could get any similar case reports of a malignant fibrothecoma with dissemination into the lymph nodes. We found a similar article of a 50-year-old postmenopausal lady with a leutinising thecoma and sclerosing peritonitis. But our patient had involvement of lymph nodes and probably even the sclerosing peritonitis which aptly explains her pain.
This was the gross macroscopic appearance of the lymph node biopsy done painstakingly by our surgery PGs but later we were appalled to learn from Pathology that the entire sample was spoilt and was unreportable as it had not been preserved in formalin.
Slide 18
So we had gone ahead with FNAC lymph node. "The FNAC is all we had but that didn't allow us to reach any conclusion if this was a metastasis of the same ovarian fibrothecoma pathology described earlier.
So we had gone ahead with FNAC lymph node. "The FNAC is all we had but that didn't allow us to reach any conclusion if this was a metastasis of the same ovarian fibrothecoma pathology described earlier.
Slide 19
With a partial diagnosis and partial relief of her pain. We wish we could have done better to relieve her pain and in the subsequent slides, I shall attempt to convey my further reading and understanding of how we may approach similar patients with terminal cancer pain.
Slide 20
Cancer pain is multifaceted which not only includes relieving the pain but has many other components of which analgesia is just one part. The other important components of pain management in such terminally ill patients are antineoplastic treatment i.e treatment of the malignant lesion itself.
Cancer pain is multifaceted which not only includes relieving the pain but has many other components of which analgesia is just one part. The other important components of pain management in such terminally ill patients are antineoplastic treatment i.e treatment of the malignant lesion itself.
Pharmacological treatment which includes analgesics and other adjuvants. Psychological and behavioural management and most importantly hospice care.
Slide 21
Now how do we asses the severity of the pain? For this, we have different scales to assess the severity of the pain like the visual analogue scale, verbal scale and numerical scale.
Now how do we asses the severity of the pain? For this, we have different scales to assess the severity of the pain like the visual analogue scale, verbal scale and numerical scale.
Slide 22
After assessment of the pain, how do we approach ahead is it just pharmacological or drugs which help in palliation? We even have the non-pharmacological modalities like various injection and neuroablative techniques and psychological interventions too.
What could actually be End of life pain in a patient who probably is at the end?
53%–70% of patients with cancer-related pain require an alternative route for opioid administration in the months and hours before death. Pain is often accompanied by other symptoms such as dyspnoea, agitation, and anxiety, any of which can exacerbate underlying central pain mechanisms. Well in our patient as to what I recall she had all of the above.
In this situation, sedation may be the only therapeutic option capable of providing adequate relief. The justification of sedation, which should bear are intervention for pain, is that it is an appropriate and proportionate goal.
Now let's see as to how we could manage her further the pain.. according to the WHO ladder for analgesia the cancer pain can be managed by categorising the pain by the severity.. For mild pain which is quite unlikely in cancer patients though, one could start initially with paracetamol and NSAIDs or a combination of both.
For pain which is between mild to moderate the choices for analgesic drugs could range from tramadol dihydrocodeine and codeine.
For severe pain, strong opioids are the option. The last Cochrane systematic review published in 2016 analysed 62 studies with 4241 participants and supported the use of oral morphine as an effective analgesic for cancer pain, with a low rate (6%) of reported intolerable adverse events. Transdermal fentanyl also achieved similar rates of effective analgesia and has also been advocated as an effective and tolerable analgesic.
With the various complexities of patients and individual variation of the cancer pain, choice of opioid is important to achieve an optimum balance between analgesia and unwanted adverse effects.
BTcP is Breakthrough cancer pain. There is no unanimous consensus on definition and characteristics of BTcP. But BTcP defined as an episode of severe pain that occurs in patients receiving a stable opioid regimen for persistent pain sufficient to provide at least mild sustained analgesia.
Now after this interpretation of BTcP could we tell that our patient was suffering from this? Well probably yes, now how could we have gone ahead in such a scenario?
Several placebo-controlled RCTs have demonstrated the efficacy of all available transmucosal fentanyl formulations for BTcP. But these products have been tested only in opioid-tolerant patients, the current recommendation is only for patients receiving doses of oral morphine equivalents of at least 60mg.
But we didn't have access to such transmucosal and intranasal fentanyl patches so we had only managed with the transdermal patch.























Comments
Post a Comment