This is a HIPAA de-identified open-online-patient-record with initial information in patient's voice, posted here after collecting informed patient consent (form downloadable Click Here) by BMJ Elective Student.
A 58-year-old man presented to the medical OP with complaints of decreased urine output since 1 day with swelling of his right knee joint since 3 days. The patient’s attendants also reported that he has been having altered behavior since the last 3 days. The patient is a resident of a city from south India and juggles between several daily wage work for his income. He is the eldest of 7 children, with 3 brothers and 3 sisters.
Detailed history of his life revealed that the patient has had palpitations since childhood, which became apparent when he was playing and when involved in any laborious tasks. Since this symptom was not incapacitating and subsided with rest, no medical attention was sought for it. The patient got married at 22 years age and subsequently had 4 children. At age 30, the patient, then working as mud digger, experienced palpitations along with shortness of breath and mild chest pain. The patient reports that these symptoms subsided with rest and hence did not seek any appropriate medical attention even then. The patient continued working, albeit with lesser intensity, now having realized that he indeed may have a health condition. He also reports that he was told by members of his family that his pulse rate was always slow (at about 40), however since his condition wasn’t incapacitating, he did not consider seeking medical attention. The patient's general physical built and other observations are captured in the images below:
The patient was a chronic smoker, smoking about 10 beedis (a form of unconventional and unfiltered cigarettes containing higher nicotine than conventional ones) a day for about 35 years and also a chronic ethanolic, consuming about 0.5 to 1L of Toddy a day for several years. He also admits to generous use of NSAIDs for generalized body aches due to heavy work. In June 2016, after a bout of heavy work, the patient had palpitations, with shortness of breath and fatigue and loss of consciousness. His Dyspnea was of sudden onset, markedly limiting physical activities and even daily activities (NYHA Gr. III). Loss of consciousness lasted for seconds, wasn’t associated with any involuntary movements of limbs, tongue biting or drooling of saliva. The patient says that he felt he was about to lose consciousness just before. He was taken to a hospital earlier. The ECG taken there is shown along with the ECG taken after pacemaker insertion (figure 1,2,3)
 |
| Figure 1 |
 |
| Figure 2 |
 |
| Figure 3 |
The ECG is showing severe Bradycardia with the heart rate calculated from R-R at 38bpm. Serial ECGs were taken and consistently showed the same finding. The patient did not have the chest x-ray taken there with him. The patient was diagnosed as a Hypertensive and was started on Atenolol 50 mg. Other investigations for renal function, liver function and routine blood tests were insignificant. A pacemaker was inserted, and the ECG is shown (Figure 1, 2, 3).
6 months after the procedure, in early January 2017, the patient gradually and progressively developed severe pain with swelling and limited range of movements in both his knees. It subsided with analgesic medication. However, the condition recurred after 3 months. TKR both knees were advised but the patient denied it. The problem kept on recurring many times, inspite of several joint aspirations. He also reports decreased urine output during these episodes. The patient did not have any reports in relation to this incident.
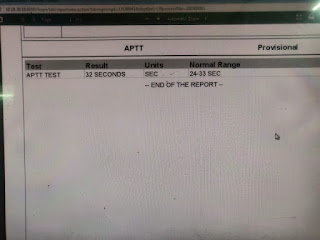
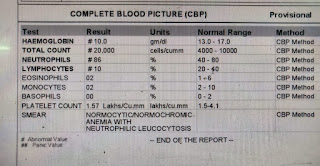
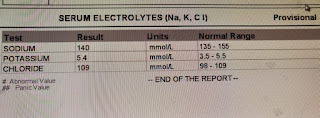
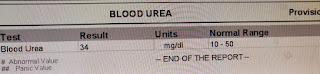
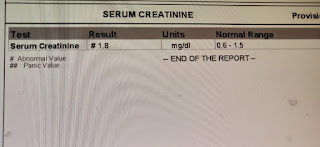
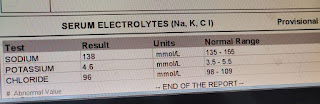
In February 2018, pain and swelling in the left knee joint subsided but increased in the right knee joint which subsided again with pain medication. On July 1st, the patient presented to our OPD with complaints of decreased urine output for 1 day and pain and swelling in the right knee joint for 3 days, with altered behavior for 3 days. He did not complain of any fever. The patient passed urine only once the day before and did not since then. Evaluation on presentation showed that the patient was irritable with a GCS of 11/15 (E3 V2 M6). A Foley’s was put and the output 400ml of high colored urine over several hours. The patient’s investigations are shared below
Acknowledgement: The history, investigations and images were collected from Dr. Aditya Samitinjay and uploaded here after deidentification



























Comments
Post a Comment